Healthcare Payment System
Insured persons or their dependents (family members) present their Myna Health Insurance Card (MYNA HOKENSHOU) or Health Insurance Eligibility Certificate at the billing counter of the healthcare provider, receive medical treatment for an illness or injury, and pay a portion of the medical care costs (out-of-pocket costs according to the percentage of the co-payment).
The healthcare provider bills each health insurance association for the remaining medical care costs (70% to 80%) through the health insurance claims review and reimbursement service (hereinafter “reimbursement service”). The health insurance association pays the medical costs to the healthcare provider through this reimbursement service.
Therefore, claims for medical expenses made to a health insurance association are handled roughly two months after the month of treatment. Insured persons receive any high-cost medical care expenses or other benefits after three months from the month of treatment.
Process of the Healthcare Payment System
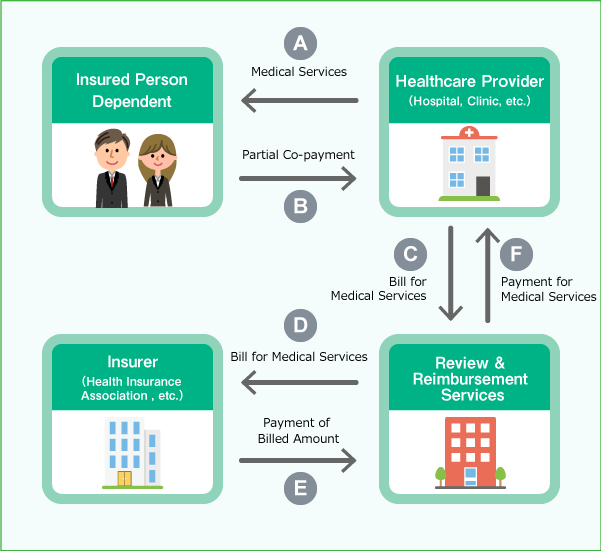
- The insured person undergoes an examination (A), presents a Myna Health Insurance Card or a Health Insurance Eligibility Certificate at the billing counter of the healthcare provider, and pays 30% of the general medical care costs after receiving treatment. (B)
- The healthcare provider bills the reimbursement service for the remaining 70% of general medical costs. (C)
- The reimbursement service reviews the statement of medical expenses (health insurance claim) submitted by the healthcare provider, and then bills the health insurance association. (D)
- The health insurance association reviews the billing statement and pays the medical costs to the healthcare provider through the reimbursement service. (E, F)